FAQ
Who founded My Medical Choice?
The founder members of My Medical Choice met in 2020.
My Medical Choice is a genuine grassroots organisation and was funded exclusively by a founder member. Funds raised go towards continuous improvements to the website, creating additional services, and supporting likeminded organisations.
Privacy is at the heart of the members’ association. Only founder members who know each other personally can hold administrative positions. This ensures confidentiality for all who join.
Unlike many other organisations, My Medical Choice guarantees that we do not harvest members’ data. We also have a policy of only emailing members when necessary – for example, when we need to update them on important matters, such as a major change to website functionality, or to send out our Newsletter.
What is My Medical Choice?
My Medical Choice is an online system of integrated healthcare services and educational material. We support members in managing their medical choices in general, and protect their healthcare wishes in emergency situations.
Why is the My Medical Choice service so crucial in the ‘Golden Hour’?
‘Golden Hour’ is a term used by emergency services and A&E staff that refers to the critical first hour immediately following a traumatic medical event. During this window of opportunity, every second counts.
As the Golden Hour includes the time spent waiting for ambulance services or helicopter medics to arrive, prompt and appropriate medical treatment is crucial to improve the chances of survival and reduce the likelihood of long-term complications or serious disability. Rapid access to accurate medical information could mean the difference between life or death.
By storing your medical history and directives online for emergency services to access, you help them avoid medical error and treat you in line with your healthcare wishes.
How this works in practice
In an emergency situation, ambulance services and pre-hospital care staff log on to our database to access a member’s emergency-contact data, healthcare history, and directives on medical procedures and treatments. Furthermore, when they log in, an SMS alert is sent to the patient’s emergency contacts (ICEs), providing them with the most important details of what has happened.
Our system’s components include:
- medical-alert jewellery tags or ID cards;
- a mobile-phone screensaver;
- optionally, a hard copy of your Advance Decision Notice (ADN).
First responders, ambulance, and A&E staff are trained to look out for these items. They gain access to your online medical profile using the login data displayed on your tag or card.
Medical data you store with us might include:
- details of any medications you are taking;
- any medical conditions you have;
- allergies or food intolerances;
- previous operations or procedures;
- any implants or devices you have had fitted;
- any medical-care directives you stipulate in our legally binding Advance Decision Notice (ADN);
- name prearranged blood donors in the event you require a blood transfusion or need blood components;
- information on Attorney(s) you have appointed to oversee treatment if you are unable to communicate after an accident or illness, in the form of a court-approved Lasting Power of Attorney document.
What is the No Blood! warning system?
Nowadays, an increasing number of people – either for religious or personal reasons - are choosing to refuse transfusions of blood and blood products. Because some paramedics are specially trained to administer blood and plasma at the scene of an accident or in the ambulance, there is a clear need for a warning system that quickly lets them know their patient does not want blood.
My Medical Choice advocates freedom of choice. We provide the following No Blood! warning system to our members:
- a No Blood! mobile-phone screensaver to download;
- the option to purchase eye-catching No Blood! medical alert tags and ID cards;
- an ADN directive stipulating that only the use of blood alternatives is acceptable;
- an ADN directive stipulating that only the use of bloodless surgery techniques is acceptable.
Non-emergency medical services
Bloodless surgery
Some of our members prefer to refuse blood and blood products. They choose to schedule operations that use alternatives to blood and plasma, combined with ‘bloodless’ surgical techniques, such as keyhole and laser surgery, for example.
To enable our members and their surgical team to get the best out of their pre-operative consultant appointment, we supply the following support documents in our Pre-op Consultation Pack:
- educational material and a Reference Library for members regarding non-blood alternatives and bloodless surgery,
- reference material for consultants regarding non-blood alternatives and bloodless surgery,
- a step-by-step guide that walks members through their appointment and prompts them to ask the right questions and encourages cooperation between patient and medical staff.
Private blood donors – an increasingly popular option
At My Medical Choice, we appreciate that some people just feel more comfortable receiving blood from someone they know, such as a family member or trusted donor from their local community. Others feel that by arranging their own private donors, they are relieving the pressure on the NHS and enabling stored blood to be used for emergencies only – especially in today’s climate when we’re told that blood stocks are often perilously low.
Alternatively, members who prefer to use private donors but do not have access to compatible family or friends may use our The National Blood Donor Database. Members can search for compatible blood donors based on postcode and region and make private arrangements between themselves and the donor.
Please note, however, that private donors are only helpful to members who require a transfusion in a non-emergency setting – such as scheduled surgery, or treatment for low haemoglobin. Private donors cannot be used in an emergency situation.
The National Blood Donor Database relies on:
- Pre-op Consultation Pack - designed specifically to use in surgical consultation appointments to support members’ wishes regarding the use of private blood donors,
- members’ blood-donor management page that helps members organise their private compatible donors.
Scotland! Although membership to My Medical Choice is applicable throughout the UK, in Scotland the legal documents have slightly different names. The Lasting Power of Attorney document is called a Welfare Power of Attorney and the Advance Decision Notice is known as an Advance Directive. For ease of use, we have referred to these documents by the names used in England and Wales.
Northern Ireland! Please note that there is no Health and Welfare Power of Attorney in Northern Ireland. Making decisions regarding the welfare of a person is the responsibility of the next of kin. Nor is an Advance Directive/Decision Notice officially recognised in law. However, even though an ADN is not officially recognised in law in Northern Ireland, if it has been completed properly the courts are likely to uphold your directives as stated in your ADN. MMC consulted the Jehovah’s Witnesses head office for advice on this matter and they have confirmed that they’ve been using their own version of an ADN in Northern Ireland for years without major issues.
What this means in practice is that you can use all the services provided by My Medical Choice except the Power of Attorney.
To compensate for not being able to appoint an Attorney, we suggest you discuss your directives for healthcare with your next of kin in great detail and ensure they understand why you wish to reject the treatments and procedures specified in your ADN before you add them as your ICE (In Case of Emergency) contact. Your named Emergency Contacts will receive the automated SMS alert provided with the service if you are involved in a medical emergency.
It may be useful to have your next of kin witness the ADN document for additional protection, as it would be difficult for them to object to the directives in your ADN in a medical emergency if they have added their details to the document and signed it.
What are the established alternatives to standard blood transfusions?
There are a number of well-established alternatives to standard NHS-donated blood transfusions available – including the possibility to opt for certain types of surgical procedures that avoid blood loss almost completely.
My Medical Choice provides members with fully referenced educational material and official NHS policy documents to help them understand their right to bodily autonomy. We also provide a reference library of studies and papers on blood alternatives, own-blood transfusions, and bloodless surgeries to present to consultants if needed.
To make the consultation appointment process as stress-free as possible, My Medical Choice members can use our Consultation Appointment Pack to learn about:
- the range of healthcare options available to them,
- how to ask the right questions of their consultant in a way that vastly increases their chance of getting the type of surgery and medical treatment that is best for them,
- how to follow up the appointment if a member and their consultant cannot reach an agreement.
The Consultation Appointment Pack also includes a PDF print-off guide to hand to the consultant or medical team during the appointment. This document gently explains our members’ stance on refusing NHS-donor blood transfusion and reminds them of patients’ rights. It also lists all the alternatives to blood transfusion that should be available to our members and informs them that, should the relevant equipment or staff expertise not be available at that hospital, then the member must be transferred to a hospital with the necessary medical equipment and experienced surgical team within the trust.
The following list gives an idea of some of the types of treatments and procedures that can be used to negate the need for a blood transfusion.
HAEMODIALYSIS
Diverts the blood into an external machine where it filters and cleans the patient’s own blood for return to the body. This procedure is suitable for members provided non-blood prime is used.
HAEMODILUTION
Diverts the blood into an external machine where it filters and cleans the patient’s own blood for return to the body. This procedure is suitable for members provided non-blood prime is used.
CELL SALVAGE MACHINES
Cell salvage technology systems, such as Hemosep, are a relatively new ultrafiltration and haemoconcentration system for concentrating residual bypass blood during or after surgery. The image below gives an idea of how these types of machine work in practice.
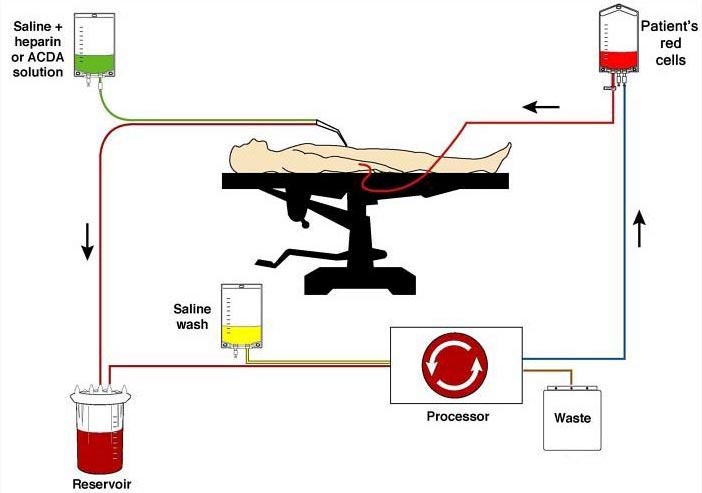 Image courtesy of Medical Illustration Department, Wythenshawe Hospital, MFT
Image courtesy of Medical Illustration Department, Wythenshawe Hospital, MFT
The image shows a continuous circuit in cell salvage, which can be requested by members.
HEART BYPASS
Diverts blood away from the heart. This procedure is suitable for members provided that non-blood prime is used.
PREOPERATIVE AUTOLOGOUS COLLECTION
Our members can also consider preoperative collection and subsequent reinfusion – although we recommend members sign and date the blood bag label to ensure chain of authenticity.
EXPANDERS
Non-blood volume expanders to ‘pad out’ blood volume can be used, such as: saline, dextran, gelatin, Ringer’s Solution, haemaccel, and hetastarch.
TRANEXAMIC ACID
This substance is used to control bleeding and helps blood to clot.
BLOODLESS SURGERY
In addition to the various choices available for alternatives to blood transfusion, members are also provided with information regarding the use of low blood-loss haemostatic surgical devices for so-called ‘bloodless surgery’.
What is a medical-alert system?
Medical-alert systems are nothing new. They’ve been used for decades to warn emergency services and A&E staff that the patient has a serious medical condition or disability, and/or is taking certain medications. They can also inform medical staff that their patient wishes to reject certain treatments, medication, or procedures (as with Jehovah’s Witnesses, for example, who refuse blood transfusions).
Medical-alert systems can be as simple as wearing a silicone band with only one word on it, such as: DIABETIC. Or they can provide more complex information printed on a medical alert jewellery tag, for example, that includes In ‘Case of Emergency’ (ICE) names and phone numbers, and login details to access online personal medical profiles.
My Medical Choice membership includes a medical-alert system that works by utilising the standard wearable medical-alert tags and ID cards but with emergency service login details printed on them. Where it differs greatly from the average medical-alert systems is in the additional use of an Advance Decision Notice (more commonly known as a living will).
Emergency services and NHS staff are trained to look out for medical-alert tags and cards/documents, meaning they can access your:
- login details to an online profile on our secure database (tag and card);
- your emergency contact’s details (ICE) such as your next-of-kin or Attorney (tag and card);
- details of allergies, medication, treatments you wish to reject, ICE details, GP contact details, a ‘pet at home alone’ alert, etc. (online medical information page and ADN)
- Optional “No Blood!” warning (tag, card, mobile-phone screensaver).
This comprehensive alert system gives medical professionals the chance to provide you with the best possible care in an emergency in line with your health directives., It also helps avoid medical error – such as adverse effects from hospital administered drugs that should not be taken with existing medication. The system also ensures staff responsible for your care are aware of any medical treatments or procedures you wish to reject, for example, a blood transfusion or invasive test.
Another useful feature of the My Medical Choice alert service is that your ICE (you can list up to two people as emergency contacts) will be sent an automated SMS alerting them to the emergency as soon as the NHS accesses your online profile, so they can come to your aid and oversee your care.
For the best possible protection, we suggest you wear your medical alert jewellery at all times, download our mobile-phone screensaver, keep your medical ID card and a copy of your Advance Decision Notice in your wallet or bag, and keep your online medical profile up to date.
What is an Advance Decision Notice (England and Wales) - Advance Directive (Scotland and Northern Ireland)?
In England and Wales, an Advance Decision Notice (ADN) is a legally-binding document that is probably better known as a ‘living will’. An ADN allows you to stipulate which medical treatments and procedures you wish to reject. It represents your voice in medical situations where you are unable to communicate.
In Scotland and Northern Ireland, an ADN is called an Advanced Directive and is not considered legally binding*. However, if one of your medical decisions were ever to be challenged in the courts, provided the Advance Directive was valid (that is, you had completed it properly and had your signature witnessed) and applicable to the circumstances (meaning the situation being raised in court was one covered by the directives you had written into your Advance Directive), it is likely a judge would rule in favour of respecting it.
One of the general principles of the Adults with Incapacity (Scotland) Act 2000 is that if someone lacks capacity to make a decision for themselves and needs medical treatment, the adult’s wishes should be taken into consideration when making a decision on their behalf; you should therefore be protected legally, since the Advance Directive allows you to stipulate your express wishes regarding your medical treatment in advance while you have the capacity to do so.
* In Northern Ireland, the relevant NHS protocol is: the Northern Ireland Pathway for the Management of Adult Patients Who Decline Specified Blood Components or Blood Products (CG424)
The My Medical Choice ADN is an easy-to-complete online form in which you simply tick the box next to the directives you choose to include on your completed ADN. Only the directives you tick will be included on your completed ADN. You can then upload your signature and that of your witness to the ADN digitally, or print it off and sign and witness it in wet ink. The hard copy can then be scanned and uploaded into your account page for emergency services to access if needed.
If you have a GP, we suggest sending them a copy using the cover letter template we provide in order to notify your GP that your ADN needs adding to your records.
Our ADN allows you to:
- tick the directives you wish to be added to the completed document – only the selected directives will appear on the final document;
- tick a “pet at home alone” warning if applicable;
- understand the implications of ticking each directive by way of pop-up information boxes where you see the information icon – – next to the directive – The information boxes include the legal/medical explanation for officially-named treatments and procedures you may wish to refuse;
- use the ADN in hard copy format, as it folds down to purse/wallet size in case a member wishes to carry it on them – perhaps while waiting for their medical alert tags or cards to arrive;
- use electronic signatures for both the member and their witnesses – although the document can also be printed off and signed in wet ink and uploaded;
- save and upload the completed ADN at the click of a button; and
- easily update the ADN digitally.
For maximum legal protection, we suggest you give a copy of your ADN to your ICE or Attorney, as well as your GP.
IMPORTANT! We suggest you review the directives in your ADN on an annual basis to ensure there’s nothing new you’d like to add or remove. You should then sign the new version (even if you make no changes to it), and send the updated copy to your GP. The online system makes this very quick and easy to do.
The annual revision of your directives and updated witnessed signature makes it difficult for anyone to argue that you have lost mental competence since your legal documents were last updated.
What is a Lasting Power of Attorney document?
A Lasting Power of Attorney (LPA), (Welfare Power of Attorney in Scotland) (WPA) is a more detailed and complex legal document than the ADN and serves a different purpose.
An LPA allows you to name one or more Attorneys* to oversee your care in the event you are not competent to make healthcare decisions, such as when unconscious after a serious accident. Once you’ve nominated an Attorney, they must uphold your wishes for medical treatment (as stipulated in your ADN).
It should be noted that the LPA has no further reach than as described and you would need to set up other types of Power of Attorney documents if you require additional protection – to deal with your property or finances, for example.
In the LPA document you are referred to as the Donor (not to be confused with blood donor), because you are ‘donating’ the responsibility for your care to an Attorney in the event you lack capacity due to an emergency. Attorneys must be over 18.
The LPA must also be witnessed (called the Certificate Provider’s Statement in the document) to state you are of sound mind, which makes it very difficult for family or medical personnel to challenge your directives later on.
Being taken to hospital (even a ‘private’ hospital) puts you firmly in the public domain, and because you will be in the public domain – whilst also at your most vulnerable - we recommend members only use the government’s version of the LPA. Members should also register their completed LPA with the appropriate court of protection for their country.
In an emergency, emergency services and A&E staff will be aware that you have an LPA document from the data you stored in our database. If they wish to verify the validity of the LPA with the court, they can do so quickly and easily. From that point on, they must take instruction from the medical directives expressed in your ADN and also your Attorney(s).
*An ‘Attorney’ in this sense, is a person who is legally appointed to make medical decisions for someone else. They require no legal or medical experience but it’s important to choose someone like-minded, trustworthy, and reliable. Your Attorney should be listed as your ICE in the medical-alert system, and you can nominate up to two Attorneys to receive the automated SMS alert in an emergency.
How can I find out what my blood type is?
If you’ve had a major operation in recent years, or given birth, your GP should have this information on your medical records, so check with them first. If you have donated blood, you are normally told your blood type about a week after donating.
What if your GP doesn’t have your blood type on record?
One option is a home test kit. It’s really quick and easy to do a finger prick test in the privacy of your own home. The most popular home testing kit is the Eldon Blood Typing Kit from ZoomHealth*.
The most professional option is to use a private medical ABO blood typing test. It is more costly, but it is something that you will only ever need to do once in your life. You will need to have a blood sample taken, which is sent off to a lab for analysis.
If you choose the ABO blood type testing, we suggest the Medichecks Blood Group Test for professional accuracy and a four-working-days turnaround time. At the time of writing, the test costs around £80, and Medichecks has a range of clinics nationwide should you need to have your blood taken by a healthcare professional.**
Please note that, whichever blood type test you use, the NHS may still insist on using their own ABO blood type test for you and your donors.
* Please note that ZoomHealth doesn’t recommend their tests be used for the purpose of blood donation. If used correctly, however, the ZoomHealth test should give you your blood type for the purpose of organising compatible donors.
** If you need to have your blood taken by a medical professional, or a nurse, there will be an additional cost depending on the option you choose.
How much medical information should I put on my profile?
It may shock you to know that in the event you are rushed into A&E, the hospital will not necessarily have medical records for you. This is because the NHS is broken up into individual trusts – usually by county. They each have their own computer system, they don’t share the information between trusts, and they can’t access each other’s records, either.
In reality, the NHS only has medical records for you if:
- you were a patient at the hospital before, and
- you provided detailed information at that time, or
- you are admitted into a hospital within the same Trust as the hospital to which you previously provided medical information.
If you have an accident in another county, the NHS has no way of accessing your records. And if you’ve never been to hospital before, the NHS can’t access your records unless you can provide GP details. This will not work if you are in hospital when your GP surgery is closed or you are unable to communicate your GP’s details.
So, you can see why a medical-alert service is a good idea!
The best way to get the most out of our service is to think of the worst-case scenario, one in which you are seriously ill or have been involved in an accident and are unconscious or unable to communicate. Then consider what information would help those caring for you to achieve the best possible outcome for your health.
The list of details below will help emergency services and A&E staff give you the most appropriate care for your needs.
- List any medical implants, such as: pacemaker, neurostimulator, aortic valve, and so on.
- List any conditions you may have: diabetes (Type 1 or 2), autoimmune conditions, COPD, asthma, etc.
- List any previous operations, or state if you have received a donated organ.
- List any serious allergies – in particular, anything that may cause anaphylaxis: peanuts, penicillin, wasp or bee stings, latex, dairy, and so on.
- List any medication or procedures you need to avoid: aspirin, ibuprofen, blood transfusions, MRI scans, invasive testing, etc.
- List medication you take regularly, including the dose and frequency (1 a day, 2 a day, etc.)
- List medication you take as and when needed: painkillers, diuretics, sleeping tablets, etc.
- List medication or devices you carry on you: steroid inhaler, EpiPen, anti-anxiety medication, etc.
And remember… if you forget to add a medication or condition to your personal medical profile, or you develop an illness and start taking medication after signing up to the My Medical Choice service, you can update your profile and legal documents as often as you need to.
Is my private data safe?
If you act responsibly with your medical-alert tag and/or ID card, then yes, your data should be quite safe.
Of course, in an emergency, emergency services access your personal health profile and ADN using the login details on your tag or card – although access is read-only. They can check the relevant medical details needed for your care, but cannot change the information they see.
Your data can only be accessed upon successful completion of a 2-step login process. This includes a unique 9-digit computer-generated passcode. The process ensures that people who know you well cannot access your data just by knowing personal details about you.
Keeping your login details safe
It is important that you take sensible precautions to keep your login details safe.
- Avoid taking off your medical-alert tag or jewellery or leaving it lying around where others can access the login details. You should wear your medical-alert jewellery at all times. It is there for your protection in an emergency. If you lose your medical-alert jewellery, change the passcode immediately to keep your data safe.
- Keep your medical ID cards safe in your purse/wallet at all times, or secure in the glove compartment of your car.
- Only share your login data with people you trust – such as your emergency contacts (ICEs) or Attorney.
What if the database is compromised?
We maintain transparency with our members, ensuring they are well-informed about the security of their data.
At My Medical Choice, the scope of personal medical information stored is significantly less comprehensive than the detailed records maintained by GPs and the NHS. Please bear in mind that extensive data is often shared with government entities and sold to private agencies. By contrast, our platform gives you control over how much data you add to your medical profile. The essential principle is to include only vital medical information that could be crucial in emergency situations to enhance the effectiveness of your care. For example, you do not need to include sensitive mental health details.
What is the National Blood Donor Database?
We set up the National Blood Donor Database in response to people who have concerns about the effect of mRNA medications on blood quality. Its purpose is to help concerned people find likeminded donors should a scheduled surgery potentially require a blood transfusion.
Ideally, members will organise their own private, compatible, on-call blood donors from among family and friends, and store their contact details in their My Medical Choice account. However, we appreciate that this option is not always possible.
We ask that members and non-members wishing to become a My Medical Choice donor add their details to the database only if they have had no mRNA-based medications or therapeutics. However, members are wholly responsible for carrying out their own due diligence before adding a donor to their trusted-donor list. To help our members stay safe, we provide them with a template mutual-trust contract to be signed by potential donors.
To enable a more harmonious relationship between member, donor(s), and the NHS, we also encourage donors to sign up to the standard Red Cross donor system (assuming they have not already) to enable their blood type to be professionally confirmed and cross-matched for antigens, and to ensure they meet the required health standards for donation. By doing so, members and their donors can remove certain barriers that may be raised when arranging private blood donation for a potential transfusion during surgery.
Why contact members from the National Blood Donor Database before you need blood?
Should a member need surgery that could involve a transfusion, it will take time to arrange a list of on-call private donors who could be accepted by the NHS. You should, therefore, begin to set up your trusted-donor list as soon as you become a member of My Medical Choice.
And there are other benefits to reaching out to potential donors straight away. Potential blood donors may be in the same situation as you and not know any like-minded people in their area. Or they may already be active in local campaign groups and happy to meet potential members for their group.
By establishing contact with donors before you need blood, you could gain the following advantages:
- peace of mind; you get a sense of how trustworthy, contactable, and reliable they are before you need them;
- if you are compatible with the donor, you may also be able to donate blood if they ever need it, which is convenient for you both;
- get to know them personally – their diet, lifestyle, health issues;
- you can broaden your horizons and meet other people like you;
- it’s a way of making friends who have similar beliefs to you regarding medical autonomy;
- if you make a friend or friends you can trust, you could arrange to be emergency contacts for each other.
But remember: safety first!
We advise our members to proceed cautiously before contacting strangers. After all, using the National Blood Donor Database is a private arrangement between members; it is used at a member’s own risk. We suggest our members read our help sheet ‘Using the National Blood Donor Database’ before using the database.
Thankfully, it is very unlikely that members will need to use the National Blood Donor Database. However, just knowing it is there gives those who want it valuable peace of mind.
Can anyone donate blood?
No. There are a number of exclusions, and the NHS provides a comprehensive list of those who should not donate blood.
Some medical conditions, cancer, for example, preclude people from donating blood, as does taking certain medications. The NHS excludes potential donors that have had a blood transfusion in the past (from 1980 onwards).
Users of the National Blood Donors Database require donors to have had no vaccines at all since mid-2018 onwards.
If in doubt, check on the NHS website to see if your medical condition(s) or the medication you are taking means you cannot give blood. The donor form gives you the option to list any conditions you may have and/or medication you take in order to give those that need blood an informed choice.
What if I have an operation scheduled where I may require blood?
For members with surgeries pending and concerns about the potential need for a transfusion, we created the Pre-op Consultation Pack. The material it contains supports them in their choices for alternatives to NHS donor blood, and educates them regarding their rights to absolute bodily autonomy. It is part of the Welcome Pack, which you can download from the Dashboard. The Pre-op Consultation Pack, which should be printed off and taken to the appointment with a copy of the member’s ADN, includes:
- Pre-op Guide for Members
- Pre-op Guide for Consultants
- The NHS policy document for patients who refuse blood
Information found in the pack includes:
- Access to an advocacy and representation helpline if things go wrong
- A follow up template document to email to the consultant in case matters are not resolved during the consultation appointment
We also provide educational help sheets and reference material to ensure our members have access to information about all the available alternatives to NHS donor blood transfusion, as well as the help sheet ‘Optimising blood for surgery’ that contains advice on how to improve overall blood health.
My Medical Choice cannot cover every possible situation and medical procedure. But we have done our best to provide members with a reasonable choice of reference material on common surgeries and treatments, and suggested a source of further information for private research.
Please note that all NHS trust CEOs have been notified that the My Medical Choice medical-alert system is currently operating in their hospitals. My Medical Choice is fully committed to helping members and NHS staff achieve the best possible outcome for all concerned in line with NHS Patient Policy.
Does this service apply in private hospitals?
Yes.
In the event of an accident, you will normally be taken to A&E. Private hospitals do not offer that facility, generally speaking, and where they do, they do not offer the service for children.
However, if you have elected to have surgery in a private hospital, you can make them fully aware of your treatment requirements in advance and allow them access to your personal health profile in case of an emergency.
You may also use the Pre-op Consultation Pack in a private consultation. Obviously, the NHS policy document would not be applicable – although your rights under the Equality Act 2010 apply to private businesses and services, too. Ask your consultant’s secretary (or applicable department) for the hospital’s terms and conditions and patient policy brochure before the consultation to give you enough time to go through it and highlight any areas of concern you may wish to discuss.
What is involved in completing my legal documents?
This is an important and detailed subject, so we’ve covered completing an Advance Decision Notice (ADN) in our FAQs, in the User Guide provided to members, and the ADN form itself contains information boxes with each directive.
The Lasting Power of Attorney (LPA) document comes with its own guide on how to complete it. With an LPA, you will be giving a great deal of power to your Attorney in the event of a serious accident or illness where you are incapacitated – so choose your Attorney(s) wisely and, before you appoint them, talk them through your wishes regarding the healthcare treatments and procedures you prefer to reject. We provide a help sheet called ‘About My Healthcare Decisions’ to help our members deal with this difficult step.
You will also need a witness to state that you are of sound mind, and separate witnesses to sign off on certain segments of the LPA. This is explained in the user guide step-by-step. Although a lengthy and comprehensive document, the LPA does NOT require legal expertise to complete and does not require the use of a solicitor. You simply fill in your personal details and arrange Witnesses to verify the details as being true.
The ADN is a much simpler document to complete, and can be signed and witnessed digitally and then printed off to use for immediate protection.
Am I able to add my children to my account?
Yes, you can. This service will be available soon.
The law throughout the UK does not allow children to use Advance Decision Notices and appoint Attorneys, and they cannot join My Medical Choice as members in their own right.
However, we are providing the option to have children’s crucial medical information added to the member parent’s account, to avoid medical error in the event of an accident. Children will need their own medical-alert tag, and their parent(s) listed as an emergency contact to ensure the parent is automatically notified if their child is admitted to hospital.
Also consider that although minors under the age of 18 cannot join My Medical Choice in their own right, they benefit from having parents that are members. Our members are well informed on patient rights regarding healthcare decisions, as well as on the laws applicable to bodily autonomy and informed consent.
What does membership to the My Medical Choice system cost?
The annual subscription is just £67 a year. Access to all the services detailed above is included and you can access and make changes to your profile and documents as often as required.
You can sign up here to begin using the service.
Medical-alert jewellery tags and ID cards
Please note that the cost of medical-alert jewellery and ID cards is not included in the subscription. The mobile-phone screensaver is available for free download to subscribers.
Although we offer links to a selection of retailers that offer a variety of suitable jewellery tags once you become a member, you are free to choose whatever medical-alert jewellery you like from any supplier you prefer. Just ensure the tag has a large enough surface to hold your login credentials – although the seller should let you know if the jewellery you have chosen is suitable before they engrave it.
The cost of medical alert jewellery varies tremendously. It really depends on your budget and whether you favour functionality or style. For example, you can choose simple coloured silicon bands that cost a couple of pounds, or choose a bespoke designer option in precious metals for a much higher cost. It is entirely up to you. Both options will do the same job.
For those on a tight budget, medical ID cards may be the better choice.
There are other accessories you can buy, such as key rings and plastic holders for your ADN, but consider that emergency services will check pulse points for necklaces and bracelets, and search purses and wallets for medical ID cards.
* My Medical Choice does not receive commission from any of the sellers listed. The sellers are suggested solely for your convenience.
Further Resources
Below you will find links to further information regarding the topics covered on this website.
Legal Documents
Advance Decision Notice (England and Wales)
Advance Directive (Scotland and Northern Ireland)
Lasting Power of Attorney (England and Wales)
Welfare Power of Attorney (Scotland)
Enduring Power of Attorney (Northern Ireland)
Refusing Blood Transfusions and Blood Components
St George’s University Hospitals Trust produced the document in this link – however, all NHS hospital trusts have very similar policies in place for refusing blood transfusions and blood products.
Children and Young Adults
Children, and Young Adults (over 16-years but under 18-years) and Consent to Treatment
Office of the Public Guardian
customerservices@publicguardian.gov.uk
Telephone: 0300 456 0300
Textphone: 0115 934 2778
Monday, Tuesday, Thursday and Friday, 9.30am to 5pm
Wednesday, 10am to 5pm
Donating Blood
Blood given via the NHS is routinely tested for: infection with hepatitis B, hepatitis C, hepatitis E, HIV, HTLV, and syphilis. Blood may also be tested for malaria or West Nile virus.
Guidelines on donating blood in Scotland
Scotland already has a system in place in which blood donors register to be on standby to give blood within 24 hours:
24-hour standby blood donation, Scotland
Who Can Give Blood?
NHS blood and transplant website
NHS Wales regulations on who can donate

